What’s New in Pancreatic Cancer Research?
Research into pancreatic cancer is under way in many medical centers throughout the world. A lot of research is focused on finding better treatments for pancreatic cancer. Improving surgery and radiation therapy are major goals, as is determining the best combination of treatments for people with certain stages of cancer.
Surgery
Surgery to remove pancreatic cancer (most often a Whipple procedure) is a long and complex operation that can be hard both for the surgeon and the patient. It often requires a long hospital stay, at least in part because of the long incision (cut) made in the belly.
A newer approach now used at some major medical centers is to do the operation laparoscopically. For this approach, the surgeon makes several small incisions in the belly instead of one large one. Long, thin surgical tools and a tiny video camera are then inserted through these cuts to do the operation. One advantage of this surgery is that people often recover from it more quickly. But this is still a difficult operation. Surgeons are looking to see how it compares to the standard operation and which patients might be helped the most by it.

* Did You Know? Each tumor is like a fingerprint, and if preserved in the right format, is essential to design more personalized treatments that are more likely to work. Hospitals do NOT preserve the tumor cells alive, and routinely discard excess tumors as medical waste. Patients have to make special arrangements to preserve their tumors at the time of surgery of biopsy.
Radiation therapy
Some studies are looking at different ways to give radiation to treat pancreatic cancer. These include intraoperative radiation therapy (in which a single large dose of radiation is given to the area of the cancer in the operating room at the time of surgery) and proton beam radiation (which uses a special type of radiation that might do less damage to nearby normal cells).
Chemotherapy
Many clinical trials are testing new combinations of chemotherapy drugs for pancreatic cancer. Many studies are seeing if combining gemcitabine with other drugs can help people live longer. Other newer chemo drugs are also being tested, as are combinations of chemo drugs with newer types of drugs.
* Did You Know? chemotherapy has many toxic side effects, and when patients are on the wrong treatment they experience severe side effects and no benefits. Chemo Sensitivity testing tests which chemotherapeutic agents works and is most effective. It prioritizes tries the choices so patients get the optimal drug. Chemo Sensitivity testing requires cancer cells be preserved alive at the time of surgery or biopsy.
Targeted therapies
Targeted drugs work differently from standard chemo drugs in that they attack only specific targets on cancer cells (or nearby cells). Targeted therapies may prove to be useful along with, or instead of, current treatments. In general, they seem to have different side effects than traditional chemo drugs. Looking for new targets to attack is an active area of cancer research.
* Did You Know? Genomic profiling, which is the test that identifies the right targeted drugs based on mutations on your tumor requires your tumor be preserved at the time of surgery or biopsy.
Growth factor inhibitors: Many types of cancer cells, including pancreatic cancer cells, have certain proteins on their surface that help them grow. These proteins are called growth factor receptors. One example is epidermal growth factor receptor (EGFR). Several drugs that target EGFR are now being studied. One, known as erlotinib (Tarceva), is already approved for use along with gemcitabine.
Anti-angiogenesis factors: All cancers depend on new blood vessels to nourish their growth. To block the growth of these vessels and thereby starve the tumor, scientists have developed anti-angiogenesis drugs. These are being studied in clinical trials for patients with pancreatic cancer.
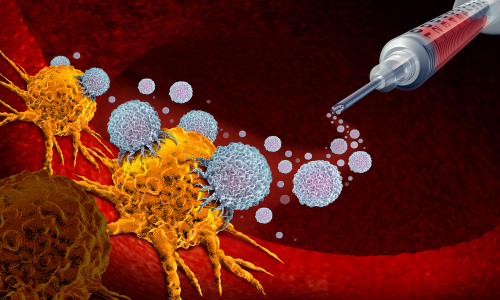
Immune therapy
Immune therapies attempt to boost a person’s immune system or give them ready-made components of an immune system to attack cancer cells. Some studies of these treatments have shown promising results.
Monoclonal antibodies: One form of immune therapy uses injections of man-made monoclonal antibodies. These immune system proteins are made to home in on a specific molecule, such as carcinoembryonic antigen (CEA), which is sometimes found on the surface of pancreatic cancer cells. Toxins or radioactive atoms can be attached to these antibodies, which bring them directly to the tumor cells. The hope is that they will destroy cancer cells while leaving normal cells alone. For use in pancreatic cancer, these types of treatments are available only in clinical trials at this time.
Cancer vaccines: Several types of vaccines for boosting the body’s immune response to pancreatic cancer cells are being tested in clinical trials. Unlike vaccines against infections like measles or mumps, these vaccines are designed to help treat, not prevent, pancreatic cancer. One possible advantage of these types of treatments is that they tend to have very limited side effects. At this time, vaccines are available only in clinical trials.
* Did You Know? personalized cancer vaccines and adoptive T cell therapy are two types of personalized cellular immunotherapy and require your tumor be preserved alive at the time of surgery or biopsy. They are both experimental, and intended to help keep patients in remission longer.
Drugs that target immune system checkpoints: The immune system normally keeps itself from attacking other normal cells in the body by using “checkpoints” – proteins on immune cells that need to be activated (or inactivated) to start an immune response. Cancer cells sometimes find ways to use these checkpoints to avoid being attacked by the immune system. Newer drugs that target these checkpoints have shown a lot of promise in treating some types of cancer. Some of these are now being studied for use in pancreatic cancer.
Individualization of therapy
Some drugs seem to work better if certain types of mutations can be found in the patient’s tumor. For example, erlotinib may work better in patients whose tumors have a particular change in the EGFR gene. This concept is an area of intense study. There might also be some gene alterations that affect how well gemcitabine will work in a particular patient. Identifying markers that can predict how well a drug will work before it is given is an important area of research in many types of cancer.
* Did You Know? preserved tumor is at the core of individualizing a treatment. What about the tumor there’s nothing to study. The tumor holds all the secrets, and when preserved in the right format, it can be studied and studied to design more tailored and effective treatments.
Don’t let anybody discard your tumor! Ironically, it can save your life.
Download more information about the latest diagnostics and immunotherapies, or schedule a free private consultation.


